Wednesday, March 05, 2008
Helicopter
I hear helicopters in the background. Not so long ago, as a child, I often looked up in excitement at the incredible speed, power and agility of such magnificent machines. Now more often than not (even when I'm not at work) I hear that engine noise and I think... work
Saturday, March 01, 2008
soaked to the skin III
Now to help the patient you have to relieve the pressure around the heart.
Usually this is (relatively) easy. You use a sternal saw and cut through the sternum. (middle of the chest where the ribs come together).
In this case it was more difficult. He's had cardiac surgery before. Which means they've already sawn (sawed?) through his sternum in the past. This is problematic because there's sometimes lots of scar tissue there now, so if you try to get in through the sternum quickly, you make have to go through scar tissue. And in that scar the patient's aorta, which is the biggest artery in the body, may be scarred together. The other option is to go in through the side of the rib cage. Since he hadn't had any surgery on his chest from the side, there's less chance of scar tissue and bleeding.
Now, the next scene is as close as you may see to a medical drama on TV. Usually as a medical professional you say "Naw that never happens!" and you criticize the accuracy of things on TV. But, now they tilt him to the side, the surgeon throws on sterile gloves, no gown, and starts cutting though the side of the chest to get to the sac around the heart. He's got blood all over his arms, he's calling to have someone page one of his partners to help him out. In the meantime, I'm giving him lots of medication to keep his heart pumping(pressors), because now it's squeezed down from the blood on the outside of it.
His partner shows up. also throws on sterile gloves, no gown. The nurses are checking blood and giving it. All of a sudden, the blood pressure shoots up to 3 times normal.... They've relieved the pressure around the heart by opening up the pericardium. Now the heart has no more pressure around it and all the medication that we're giving to help the heart squeeze is working too....
But now there's bleeding all around the heart... they need to look for the hole that caused the blood to escape the heart and fill up the pericardial sac in the first place. It's dark in the EP lab, because most of the procedures are done looking at video monitors. Even with all the lights on it's dark in there. At this point they've fillup a whole suction container with blood (1.5 liters) we're giving blood. they're a good way towards filling a second. He asks for a certain kind of stitch... of course they don't have it in EP lab. Why would they need a cardiac surgery stitch. he puts his finger over what he thinks is the hole and yells to have them call up to the OR and get the stitches he needs. I yell to have them call up also and have them get a cardiac OR ready. I assume we'll need to go up there eventually, if we make it.
He finally gets the stitch he needs... puts in a couple more.... still bleeding from around the heart, now there's some bleeding from there entry into the chest too. "I don't know how we're gonna get this guy upstairs" he says. A couple of more stitches, some more blood given, more pressors given. he finally decides that he's got some marginal control of the bleeding and to pack some pads around the heart, to hopefully place pressure on the hole and give us a chance to get up to the OR where the proper equipment and help can be used. The pads go in, 2 stitches to hold the rib cage closed, and a big sheet of sticky plastic (think medical grade iodine impregnated contact paper) to keep the area, marginally clean. I'm a bit surprised we've managed to keep him alive this far.
We roll the patient over to get him over to a stretcher. This is what starts the soaking of my clothes. we get him moved over. we rush to the elevator and up to the OR. It takes several minutes to get up there, we're giving blood and pressors like crazy. we need to position the patient on the side more properly so he has better access to the side of the chest than he did downstairs.
I help roll the patient again, i'm leaning over the wound and it's starting to well up around the plastic sheet. now it's leaking over me, warm. I can't stop, because I know this guy's going to die, and I can't let it be my fault. We finally get organized and they're prepping the patient to go back into the chest.
we're sort of stable now on lots of pressors, but giving a little less blood... until they open up the plastic.... blood starts gushing out again. we scramble a bit. One of the other cardiac anesthesiologists shows up, asks if I need a hand. I ask him if he can help the residents out so I can change.
I scurry down the hall, my belly and crotch covered mostly in blood. I must be a sight. I go to my office, take my scrubs off, my underwear is bloody too. yuk. Luckily I have a clean pair if my office (for call nights) I go wash my hands and I'm back in the OR.
Twenty minutes later, the surgeons can't find the hole, and they're bleeding from all around the heart and incision and multiple transfusions and medications later the man's 80+ year old heart gives up.
I ask the resident if she's okay to tidy on her own and we all walk out of the operating room defeated.
Unfortunately we can't win them all.
Usually this is (relatively) easy. You use a sternal saw and cut through the sternum. (middle of the chest where the ribs come together).
In this case it was more difficult. He's had cardiac surgery before. Which means they've already sawn (sawed?) through his sternum in the past. This is problematic because there's sometimes lots of scar tissue there now, so if you try to get in through the sternum quickly, you make have to go through scar tissue. And in that scar the patient's aorta, which is the biggest artery in the body, may be scarred together. The other option is to go in through the side of the rib cage. Since he hadn't had any surgery on his chest from the side, there's less chance of scar tissue and bleeding.
Now, the next scene is as close as you may see to a medical drama on TV. Usually as a medical professional you say "Naw that never happens!" and you criticize the accuracy of things on TV. But, now they tilt him to the side, the surgeon throws on sterile gloves, no gown, and starts cutting though the side of the chest to get to the sac around the heart. He's got blood all over his arms, he's calling to have someone page one of his partners to help him out. In the meantime, I'm giving him lots of medication to keep his heart pumping(pressors), because now it's squeezed down from the blood on the outside of it.
His partner shows up. also throws on sterile gloves, no gown. The nurses are checking blood and giving it. All of a sudden, the blood pressure shoots up to 3 times normal.... They've relieved the pressure around the heart by opening up the pericardium. Now the heart has no more pressure around it and all the medication that we're giving to help the heart squeeze is working too....
But now there's bleeding all around the heart... they need to look for the hole that caused the blood to escape the heart and fill up the pericardial sac in the first place. It's dark in the EP lab, because most of the procedures are done looking at video monitors. Even with all the lights on it's dark in there. At this point they've fillup a whole suction container with blood (1.5 liters) we're giving blood. they're a good way towards filling a second. He asks for a certain kind of stitch... of course they don't have it in EP lab. Why would they need a cardiac surgery stitch. he puts his finger over what he thinks is the hole and yells to have them call up to the OR and get the stitches he needs. I yell to have them call up also and have them get a cardiac OR ready. I assume we'll need to go up there eventually, if we make it.
He finally gets the stitch he needs... puts in a couple more.... still bleeding from around the heart, now there's some bleeding from there entry into the chest too. "I don't know how we're gonna get this guy upstairs" he says. A couple of more stitches, some more blood given, more pressors given. he finally decides that he's got some marginal control of the bleeding and to pack some pads around the heart, to hopefully place pressure on the hole and give us a chance to get up to the OR where the proper equipment and help can be used. The pads go in, 2 stitches to hold the rib cage closed, and a big sheet of sticky plastic (think medical grade iodine impregnated contact paper) to keep the area, marginally clean. I'm a bit surprised we've managed to keep him alive this far.
We roll the patient over to get him over to a stretcher. This is what starts the soaking of my clothes. we get him moved over. we rush to the elevator and up to the OR. It takes several minutes to get up there, we're giving blood and pressors like crazy. we need to position the patient on the side more properly so he has better access to the side of the chest than he did downstairs.
I help roll the patient again, i'm leaning over the wound and it's starting to well up around the plastic sheet. now it's leaking over me, warm. I can't stop, because I know this guy's going to die, and I can't let it be my fault. We finally get organized and they're prepping the patient to go back into the chest.
we're sort of stable now on lots of pressors, but giving a little less blood... until they open up the plastic.... blood starts gushing out again. we scramble a bit. One of the other cardiac anesthesiologists shows up, asks if I need a hand. I ask him if he can help the residents out so I can change.
I scurry down the hall, my belly and crotch covered mostly in blood. I must be a sight. I go to my office, take my scrubs off, my underwear is bloody too. yuk. Luckily I have a clean pair if my office (for call nights) I go wash my hands and I'm back in the OR.
Twenty minutes later, the surgeons can't find the hole, and they're bleeding from all around the heart and incision and multiple transfusions and medications later the man's 80+ year old heart gives up.
I ask the resident if she's okay to tidy on her own and we all walk out of the operating room defeated.
Unfortunately we can't win them all.
Labels:
black cloud,
blood blood blood,
electrophysiology,
on call,
tamponade
Monday, February 18, 2008
soaked to the skin II
anyway, sorry for the delay.. where was I...
So they're doing CPR on the patient. I went up to the anesthesiologist and asked what was going on. Apparently they were doing an ablation in the ventricle and they had starting getting low blood pressure during the case, then a cardiac arrest.
Now you see some people have irregular rhythms in their hearts. Usually these are cause for little areas of abnormal tissue in the heart, they can burn these areas and usually the irregular rhythms will go away. This is called an ablation. Sometimes they burn through too much and they can get into trouble. It's known to happen, but usually rare.
The problem they have here is now they have a hole in the heart and it starts to bleed. That in and of itself isn't great, but the main problem is that the heart sits in a little sac of tissue called the pericardium (literally "around the heart"). Once it's full of blood, if you have continued bleeding it starts to compress the heart and the compressed heart can no longer fill and pump blood. This causes low blood pressure and eventally cardiac arrest. This is called cardiac tamponade. The way to fix this is to open up the pericardial sac and let the blood from around the heart out, then it can again fill and pump blood. The problem with this is that you still have bleeding and now it's not just limited to the pericardium, but can continue to bleed.
More later...
So they're doing CPR on the patient. I went up to the anesthesiologist and asked what was going on. Apparently they were doing an ablation in the ventricle and they had starting getting low blood pressure during the case, then a cardiac arrest.
Now you see some people have irregular rhythms in their hearts. Usually these are cause for little areas of abnormal tissue in the heart, they can burn these areas and usually the irregular rhythms will go away. This is called an ablation. Sometimes they burn through too much and they can get into trouble. It's known to happen, but usually rare.
The problem they have here is now they have a hole in the heart and it starts to bleed. That in and of itself isn't great, but the main problem is that the heart sits in a little sac of tissue called the pericardium (literally "around the heart"). Once it's full of blood, if you have continued bleeding it starts to compress the heart and the compressed heart can no longer fill and pump blood. This causes low blood pressure and eventally cardiac arrest. This is called cardiac tamponade. The way to fix this is to open up the pericardial sac and let the blood from around the heart out, then it can again fill and pump blood. The problem with this is that you still have bleeding and now it's not just limited to the pericardium, but can continue to bleed.
More later...
Labels:
anesthesia,
blood blood blood,
electrophysiology,
on call,
tamponade
Thursday, February 07, 2008
soaked the skin
As an anesthesiologist you shouldn't need to go to your office and change your scrubs in the middle of a case.
No I didn't soil myself because the case scared the heck out of me because it did, but I was covered in blood from moving the patient on to the bed.
I'm on call today and I was headed down to the Electropysiology (EP) lab to relieve the anesthesiologist down there so he could go home. I'm poking around looking to find out which room he's in. I pop my head in one room, I see a CRNA... have you seen Dr. X? Oh he was just here but he's probably next door... they're having trouble.
Hmm... that's not a good sign. I go into the room and usually the room is dark and quiet, the patient is on the bed under light sedation... they're usually pretty sick, but generally unexciting. Anyway... I go into the room, there's a ton on noise and they're doing chest compressions (CPR) A cardiac surgeon is standing near the bedside and they're pulling out surgical equipment.
(More later)
No I didn't soil myself because the case scared the heck out of me because it did, but I was covered in blood from moving the patient on to the bed.
I'm on call today and I was headed down to the Electropysiology (EP) lab to relieve the anesthesiologist down there so he could go home. I'm poking around looking to find out which room he's in. I pop my head in one room, I see a CRNA... have you seen Dr. X? Oh he was just here but he's probably next door... they're having trouble.
Hmm... that's not a good sign. I go into the room and usually the room is dark and quiet, the patient is on the bed under light sedation... they're usually pretty sick, but generally unexciting. Anyway... I go into the room, there's a ton on noise and they're doing chest compressions (CPR) A cardiac surgeon is standing near the bedside and they're pulling out surgical equipment.
(More later)
Labels:
anesthesia,
black cloud,
blood blood blood,
electrophysiology,
on call
Tuesday, January 29, 2008
Stat!
"Staff Stat to OR Z"
Hmm.... not good. usually.
This is an alarm system we have so if there's anesthesia emergency and the staff is not in the room, the resident or a nurse can call overhead on the speakers and everyone available can come to the room to help whomever is in there.
Sometimes it's only a false alarm, the patient's oxygen level is reading a little low and the resident gets a little worried.
Sometimes it's much worse.
"Staff stat to OR Z"
I shuffle quickly over there.
I walk in, they are doing chest compressions. Apparently the patient "crashed" about 10 minutes after the start of the case.... low blood pressure of uncertain origin, didn't improve with treatment at all so they started CPR (Cardio Pulmonary Rescusitation). Emergency drugs were given.... epinephrine, atropine, all the good stuff.
After about 15 more minutes after I arrived, they called it, meaning they pronounced the patient dead, all attempts unsuccessful to resuscitate failed. The anesthesia staff in charge of the case don't know what the issue was... the patient was "relatively" healthy. Definitely will need an autopsy to see if anything obvious shows up.
Anyway, we all shuffle out, mostly feeling defeated a little.
Ten minutes later,
"Staff stat to OR 10"
Weren't we just in there?
I head back over there. They're doing chest compressions again.... apparently they were cleaning up the room and filling out the death packet and they saw some rhythm on the monitor so they felt they should give it another shot. Although in the meantime, they hadn't been ventilating the patient or watching the patient since she were pronounced dead. (why would they?)
We persisted a few minutes and then we all decided that it was probably futile... some sort of agonal near death heart reflex (which often happens).
We all left the room again... though not before I disconnected the monitor.
Sadly we can't win them all.
Hmm.... not good. usually.
This is an alarm system we have so if there's anesthesia emergency and the staff is not in the room, the resident or a nurse can call overhead on the speakers and everyone available can come to the room to help whomever is in there.
Sometimes it's only a false alarm, the patient's oxygen level is reading a little low and the resident gets a little worried.
Sometimes it's much worse.
"Staff stat to OR Z"
I shuffle quickly over there.
I walk in, they are doing chest compressions. Apparently the patient "crashed" about 10 minutes after the start of the case.... low blood pressure of uncertain origin, didn't improve with treatment at all so they started CPR (Cardio Pulmonary Rescusitation). Emergency drugs were given.... epinephrine, atropine, all the good stuff.
After about 15 more minutes after I arrived, they called it, meaning they pronounced the patient dead, all attempts unsuccessful to resuscitate failed. The anesthesia staff in charge of the case don't know what the issue was... the patient was "relatively" healthy. Definitely will need an autopsy to see if anything obvious shows up.
Anyway, we all shuffle out, mostly feeling defeated a little.
Ten minutes later,
"Staff stat to OR 10"
Weren't we just in there?
I head back over there. They're doing chest compressions again.... apparently they were cleaning up the room and filling out the death packet and they saw some rhythm on the monitor so they felt they should give it another shot. Although in the meantime, they hadn't been ventilating the patient or watching the patient since she were pronounced dead. (why would they?)
We persisted a few minutes and then we all decided that it was probably futile... some sort of agonal near death heart reflex (which often happens).
We all left the room again... though not before I disconnected the monitor.
Sadly we can't win them all.
Friday, January 18, 2008
Computers down!
Went to a doctors appointment today. I usually go at 8am. The doctors tend to run behind and if I'm the 1st patient of the day they can't be behind. Anyway, the doors are usually unlocked at 7:45 or so. I pull up and there are three or four people milling around the door. At about 8 they open the door. I walk in and try to check in. Apparently the computers and phones were down. They couldn't check me in, they couldn't put me in a room. Fifteen minutes later, they put me in a room and found some forms to manually check me in. The doctor comes in a few minutes later, he's obviously flustered.
How are you doing? Did they check your sugar today? No of course not, the computer would have told them to do that. Sorry we have no chart, we're all paperless now. What was your last Hgb A1C? your memory is better than mine... an altogether unsettling visit. He's a really good doctor and actually remembered a lot off the top of his head.
Funny how relient we are on computers in the medical field these days. I know I couldn't do my job very well without a computer
Oh, Happy New Year
Sunday, December 09, 2007
Sick
It's that time of year again. Time for flu, colds, etc.
I was in charge of making sure rooms in our building were assigned to residents and faculty the other day. This includes assigning where add on cases go and making sure people get breaks and lunches and relieved at the end of the day.
One of the residents came up to me and told me he might need extra breaks because he's been having some "GI (gastrointestinal) problems" and been running to the bathroom. He said he was probably going to the emergency room after work because it had been going on for five days or so.
Yikes! A few minutes later his faculty came up to me and said his resident looked terrible and diaphoretic (sweaty) and should be sent home. I agreed and called over to the main building to see if there was someone extra to send over.
I went to his OR and told him we were sending someone over to relieve him. He protested and wanted to stay. "This is an interesting case, and I need my vascular cases"
I said, "If you need to go to the ER after work, you need to go to the ER now. You can't get your vascular cases if you fall over. You can always come back if you're okay"
He finally agreed and he was sent home. I think he didn't need to be admitted to the hospital, but earned himself a CT scan and lots of blood tests.
A couple days later, a (different) resident popped into my office.
"You in charge?"
"No, why"
"I just threw up I think i need to go home"
"Fair enough Dr. X is in charge... he just walked past here"
I went out to the break area a few minutes later.
I overheard, "X looked terrible"
"I heard she threw up"
"She must be pregnant"
Laughter from the guys. "No think she's actually sick, she looks terrible"
She walked back by, looking annoyed "I'm NOT pregnant"
I was in charge of making sure rooms in our building were assigned to residents and faculty the other day. This includes assigning where add on cases go and making sure people get breaks and lunches and relieved at the end of the day.
One of the residents came up to me and told me he might need extra breaks because he's been having some "GI (gastrointestinal) problems" and been running to the bathroom. He said he was probably going to the emergency room after work because it had been going on for five days or so.
Yikes! A few minutes later his faculty came up to me and said his resident looked terrible and diaphoretic (sweaty) and should be sent home. I agreed and called over to the main building to see if there was someone extra to send over.
I went to his OR and told him we were sending someone over to relieve him. He protested and wanted to stay. "This is an interesting case, and I need my vascular cases"
I said, "If you need to go to the ER after work, you need to go to the ER now. You can't get your vascular cases if you fall over. You can always come back if you're okay"
He finally agreed and he was sent home. I think he didn't need to be admitted to the hospital, but earned himself a CT scan and lots of blood tests.
A couple days later, a (different) resident popped into my office.
"You in charge?"
"No, why"
"I just threw up I think i need to go home"
"Fair enough Dr. X is in charge... he just walked past here"
I went out to the break area a few minutes later.
I overheard, "X looked terrible"
"I heard she threw up"
"She must be pregnant"
Laughter from the guys. "No think she's actually sick, she looks terrible"
She walked back by, looking annoyed "I'm NOT pregnant"
Friday, November 23, 2007
Shock of your life
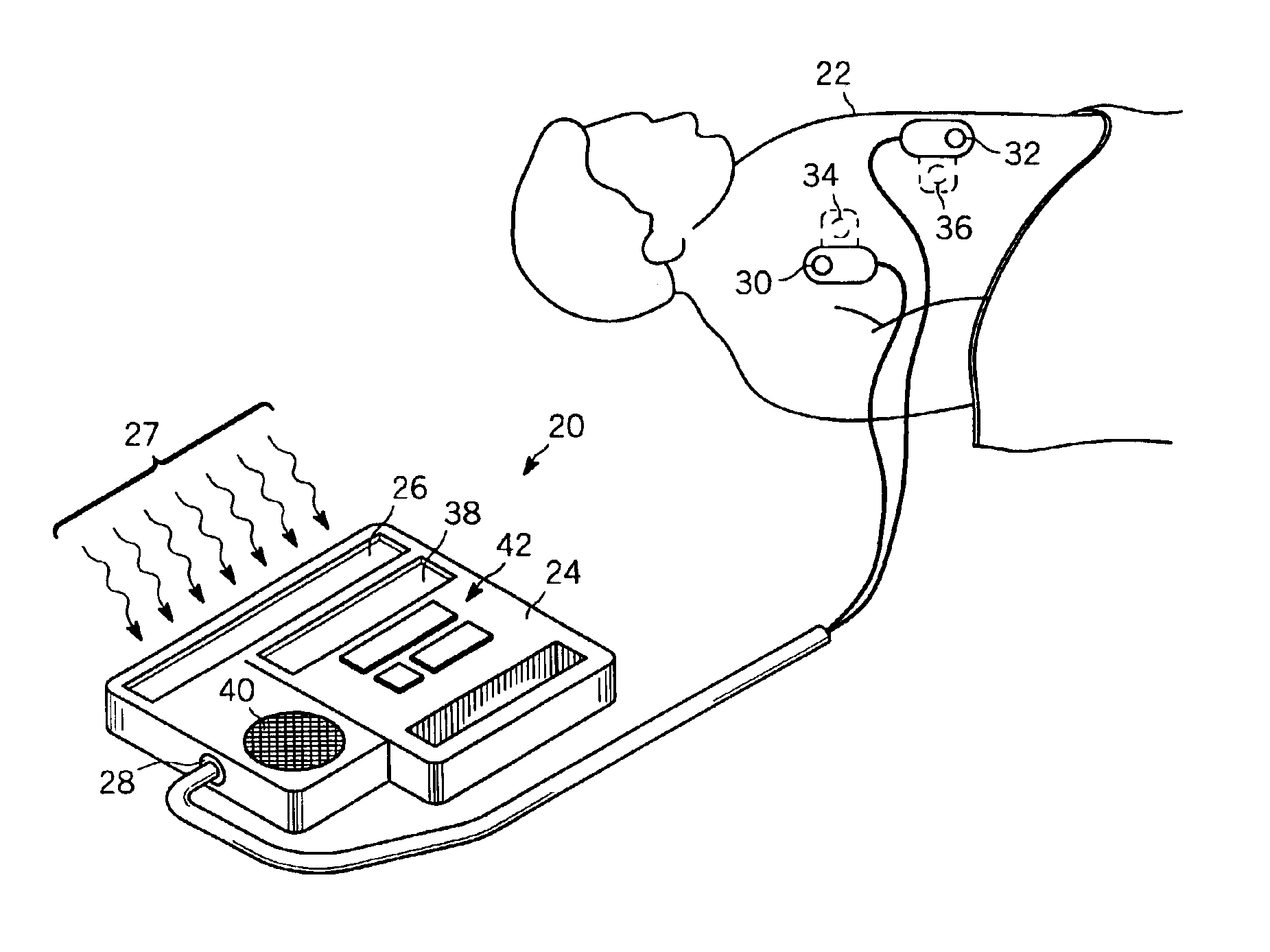
Image used without permission from freepatentsonline.com
I'm staffing a case down in the Electophysiology (EP) lab. Here is where the cardiologists look at the heart from the inside and do various procedures to help fix conduction abnormalities in the heart. They implant defibrillators and pacemakers in the EP labs.
There was a young man on the table, we were getting ready to sedate him for a procedure for an irregular heartbeat. Our anesthesia monitors were being put on and I was looking at the chart. All of a sudden I saw the patient jump up... I thought he was trying to crawl off the bed. Then someone started apologizing....
Apparently she was testing the external defibrillator. This is the device used to put a shock through a patient's chest to put it his/her heart back into a regular rhythm if it goes into a dangerous rhythm. You see this all the time on ER and Grays Anatomy and such. Anyway during this procedures where we are trying to cure these rhythms there is a high likely hood of putting a patient into one of these dangerous rhythms. So as a precaution they always have the external defibrillator in the room and two electrode patches on the patient. In this case during the test of the device someone had already hooked it up to the patient. So this patient got quite a nasty shock. He shook his head like he was stunned and said he was alright three or four times... all the staff were really apologetic.
This would have been a little amusing to me except for the fact that when a person is in a "normal" heart rhythm, shocking them may put them into a dangerous one that is life threatening.
Glad it wasn't me though
Labels:
anesthesia,
defibrillator,
electophysiology,
ep,
shock
Friday, October 12, 2007
Neck mobility
I was in preop anesthesia clinic yesterday. I saw a patient that had been in a car accident and had his neck fused c2-c5 (I believe) and he had very little neck movement at all.
In anesthesia there are markers to predict or at least suggest it may be difficult to place a breathing tube in someone. These include mouth opening, dentition, mallampatti score, which assesses the favorablity of the anatomy of the oral cavity (i.e. mouth), hyoid to mentum distance (essentially chin size), neck thickness/anatomy, neck extension and flexion. No one predictor predicts a difficult intubation, but together they form a picture of how easy or difficult you think it might be.
Someone with very limited neck movement would be very difficult to visualize the vocal cords generally, so I was worried a bit in this case. Apparently he had had two surgeries in the past six months with no problems and the anesthesiologists had not told him anything about his airway. So just to be sure I requested the anesthesia record from the other hospital.
It was your standard anesthesia record, with lots of checkboxes for standard things that you do in the operating room.
Easy mask ventilation - checkmark -- reassuring because that means you can still mask ventilate if you happen to have trouble intubating.
Iv induction - checkmark.
Easy intubation - checkmark
Mac 3 - checkmark
2nd attempt - checkmark
Blind intubation - checkmark
whoa.... wait a minute. it was an easy intubation, but he/she wasn't able to visualize the vocal cords?
So now I flip through the rest of the records... no note about the airway at all, or being difficult or anything. I have to now doubt the accuracy of this whole chart now.... How can I trust that he was a easy mask ventition if she/he was willing to describe the blind intubation is easy.
Enough to drive you crazy.
In anesthesia there are markers to predict or at least suggest it may be difficult to place a breathing tube in someone. These include mouth opening, dentition, mallampatti score, which assesses the favorablity of the anatomy of the oral cavity (i.e. mouth), hyoid to mentum distance (essentially chin size), neck thickness/anatomy, neck extension and flexion. No one predictor predicts a difficult intubation, but together they form a picture of how easy or difficult you think it might be.
Someone with very limited neck movement would be very difficult to visualize the vocal cords generally, so I was worried a bit in this case. Apparently he had had two surgeries in the past six months with no problems and the anesthesiologists had not told him anything about his airway. So just to be sure I requested the anesthesia record from the other hospital.
It was your standard anesthesia record, with lots of checkboxes for standard things that you do in the operating room.
whoa.... wait a minute. it was an easy intubation, but he/she wasn't able to visualize the vocal cords?
So now I flip through the rest of the records... no note about the airway at all, or being difficult or anything. I have to now doubt the accuracy of this whole chart now.... How can I trust that he was a easy mask ventition if she/he was willing to describe the blind intubation is easy.
Enough to drive you crazy.
Thursday, October 11, 2007
Perioperative Guidelines
Got sent the new ACC/AHA revised perioperative cardiovascular guidelines for non-cardiac surgery. It was a PDF attached to my email, and I figured I should know what's in them since I work in the preop anesthesia clinic, so I printed them out...what could it be... ten pages maybe...
nope.
I went to the printer and it was still printing and it was neverending.
82 pages!
Yikes... I know it's a complex topic, and I need to know them.
6 pages down... 76 more to read... i think some of them are references though... maybe only 70 pages...
nope.
I went to the printer and it was still printing and it was neverending.
82 pages!
Yikes... I know it's a complex topic, and I need to know them.
6 pages down... 76 more to read... i think some of them are references though... maybe only 70 pages...
Wednesday, October 03, 2007
Hand Sanitizer

Image used without permission from childrenshospital.org
Just got a message on my pager.
I accidentally contaminated the sterile field with [brand deleted hand sanitizer] ( that went out of control) --[resident name deleted]
Our hospital has gone to having alcohol based hand sanitizer everywhere, to decrease the spread of infection... there's one on the side of the anesthesia cart. Apparently, the spout had gotten clogged a bit and when she went to pump some on her hands it squirted sideways and hit two people scrubbed-in and the corner of the instrument table... and we're doing a descending thoracic aneurysm repair and they're often super-paranoid (rightfully) so that the artificial graft material doesn't get infected.
Didn't seem the surgeon had flipped out though... probably due to the fact that it's 62% alcohol and probably made the surgical field cleaner.
You can't make this stuff up.
Friday, September 28, 2007
Locked out
I was on call yesterday and there was a fire drill going on so the fire alarms were going off... i was headed to the ORs to wake up a patient with one of the residents and I swiped my ID at the OR doors... Nothing... no click, just blinking lights on the pad. I swiped my ID again. Same. So I pulled on the door. still locked no way to open it. Luckily someone was exiting the locker room and I got in there and cut into the ORs. This happened on one other occasion with a different door soon after the opening of our new addition, which I chalked up to being in a new building. I don't know if this is the case with any other doors, but I'm guessing it is.
This is a serious problem. Luckily I was going to a routine wake-up with a good resident and I wasn't really needed. But we need to get into the ORs, or really anywhere in the hospital where we are needed regardless of whether a fire drill is happening or not, or a real fire, or if the building is falling down. This goes the same for the residents who may be running to a code or emergent airway.
Excuse me while I spend the next half hour composing a coherent email to the higher-ups
Monday, September 24, 2007
Fat
Wow.
One of my rare days now where I'm not doing cardiac or thoracic cases.
The patient had a Body Mass Index (BMI= weight in kg/ [height in meters]squared) of 78! Overweight is above 25, obese above 30. It's a little conservative in my opinion, but this is ridiculous. He was 5 foot 6 or so, and above 220kg. (~500 lbs) fortunately he was here for gastric bypass surgery.
When they're this big, you worry if you're able to get IV access, establish the airway, and whether the surgeons will have difficulty with the procedure.
Anyway, after we put the patient to asleep and intubated him the attending surgeon asked:
"How did you know that would be easy?"
My reply, "I didn't."
I moved along into how we examine the patient and the markers we look for that predict difficulty (or lack thereof)
Luckily no problems.
I did have salad for lunch... I need to work on my own BMI.
One of my rare days now where I'm not doing cardiac or thoracic cases.
The patient had a Body Mass Index (BMI= weight in kg/ [height in meters]squared) of 78! Overweight is above 25, obese above 30. It's a little conservative in my opinion, but this is ridiculous. He was 5 foot 6 or so, and above 220kg. (~500 lbs) fortunately he was here for gastric bypass surgery.
When they're this big, you worry if you're able to get IV access, establish the airway, and whether the surgeons will have difficulty with the procedure.
Anyway, after we put the patient to asleep and intubated him the attending surgeon asked:
"How did you know that would be easy?"
My reply, "I didn't."
I moved along into how we examine the patient and the markers we look for that predict difficulty (or lack thereof)
Luckily no problems.
I did have salad for lunch... I need to work on my own BMI.
Tuesday, September 18, 2007
Sad
I pulled out my bike from the garage yesterday to ride it to the gas station to get some air for the tires... It's about two miles I guess. Anyway, I was recounting this to my girlfriend who seemed glad I was getting some exercise.
"Well it took you about 30 minutes... that's not too bad."
"Minus stopping for air..."
"You were that winded?"
"... Air... for the tires."
I must be more out of shape than I thought.
"Well it took you about 30 minutes... that's not too bad."
"Minus stopping for air..."
"You were that winded?"
"... Air... for the tires."
I must be more out of shape than I thought.
Thursday, September 06, 2007
Poop
Luckily my friend's dad is feeling a bit better... kicked out of the hospital. No more obsession with flatus. Now family is obsessed with poops.
Tuesday, September 04, 2007
Abdominal surgery
My friend's father had emergency bowel surgery this past weekend, so I've received many surgical type questions which I'm marginally qualified to answer. In any case I'm finding it amusing with how my attention is being taken to his gastrointestinal tract, specifically the ability to pass gas. Hope he's feeling better soon.
Friday, July 27, 2007
Mini Mall
Ever heard of grand mal seizures? It's the type of seizures most think about as seizures, with unconsciousness and violent jerking movements.
I'm in clinic today. On her history form she has written "mini mall seizures".
I usually shop at mini-malls, but I think she means petit-mal seizures. These are also known as absence seizures and not associated with jerking motions.
I'm in clinic today. On her history form she has written "mini mall seizures".
I usually shop at mini-malls, but I think she means petit-mal seizures. These are also known as absence seizures and not associated with jerking motions.
Monday, July 16, 2007
Poor historian
I'm in clinic again... the bane of the non-pain anesthesiologist. A 60-some year old woman is here for surgery. She's had a history of heart failure. (Her heart is damaged so it doesn't pump very efficiently) She's a terrible historian.
Now for non-medical types, this doesn't mean she didn't know that Washington crossed the Delaware. It means that she's a terrible reporter of her own medical history. For different patients it means different things. To some it means that they can't remember what they've had done in the past or what medical conditions they have. To others it means that they ramble on so much it's hard to separate the medical information from random stories about their puppy. And my favorite group is the group where they're so vague about things that it takes 14 follow-up questions to get what you want from them.
"So how bad has your heart failure been" (Looking at the chart with 6 heart failure meds on.)
"Oh I don't really have heart failure"
"Hmm... really. Can you climb a flight of stairs?" (I don't care if she has stairs in her house, I just want to know if she can tolerate minor exercise)
"Oh I don't really climb stairs with my back and all" (Meaning she can't do it)
"How about walking, how far can you walk?" (Easier than stairs)
"Oh not far..."
"Do you ever get chest pain or shortness of breath?"
"Well not really.... well only if I walk too far." (Meaning yes all the time)
(inside) *sigh*
So I look again through the notes. There's a note from the Primary care provider (PCP) "Will stress before surgery." Now someone there has a good idea. Good to know if this lack of function is due to her heart or her back before we possibly kill her in the operating room.
I flip to the studies. I see a non-stress echocardiogram (essentially a heart ultrasound picture) from five months ago showing diastolic dysfunction. And a stress echocardiogram (same pictures, but while giving a chemical to stress the heart) from last month. "Indeterminate. Study cancelled due to hypertensive response." So they cancelled the stress in the middle because her blood pressure got too high. Fine. What did they do about that. I see another non-stress echocardiogram from two weeks ago. Hmm.... curious. So the stress was unable to be done, so they repeated a test that DIDN'T stress the heart, and had results we ALREADY knew about.
So it's six days til her surgery, I have a patient with known heart failure, maybe shortness of breath, maybe chest pain, two non-stress tests, and an indeterminate stress test. Someone also has decided before me that a stress would be a good idea, but never really followed through. So I have six days (including two weekend days) to get her stressed (a different type of stress test) or cancel the surgery. Luckily the ladies out front (the wonderful office staff) are able to get her scheduled for early next week. I cross my fingers and let her go.
The intern asks me what happens if the stress is positive next week. Good question. If it's negative, then I'm just a worry-wort and paranoid about nothing but she should get her back fixed. If not, then they need to evaluate her to see if anything can be done to optimize her heart before her elective surgery. This may mean changing her medications, or performing a heart catheterization, or more.
Did I tell you I love clinic?
Now for non-medical types, this doesn't mean she didn't know that Washington crossed the Delaware. It means that she's a terrible reporter of her own medical history. For different patients it means different things. To some it means that they can't remember what they've had done in the past or what medical conditions they have. To others it means that they ramble on so much it's hard to separate the medical information from random stories about their puppy. And my favorite group is the group where they're so vague about things that it takes 14 follow-up questions to get what you want from them.
"So how bad has your heart failure been" (Looking at the chart with 6 heart failure meds on.)
"Oh I don't really have heart failure"
"Hmm... really. Can you climb a flight of stairs?" (I don't care if she has stairs in her house, I just want to know if she can tolerate minor exercise)
"Oh I don't really climb stairs with my back and all" (Meaning she can't do it)
"How about walking, how far can you walk?" (Easier than stairs)
"Oh not far..."
"Do you ever get chest pain or shortness of breath?"
"Well not really.... well only if I walk too far." (Meaning yes all the time)
(inside) *sigh*
So I look again through the notes. There's a note from the Primary care provider (PCP) "Will stress before surgery." Now someone there has a good idea. Good to know if this lack of function is due to her heart or her back before we possibly kill her in the operating room.
I flip to the studies. I see a non-stress echocardiogram (essentially a heart ultrasound picture) from five months ago showing diastolic dysfunction. And a stress echocardiogram (same pictures, but while giving a chemical to stress the heart) from last month. "Indeterminate. Study cancelled due to hypertensive response." So they cancelled the stress in the middle because her blood pressure got too high. Fine. What did they do about that. I see another non-stress echocardiogram from two weeks ago. Hmm.... curious. So the stress was unable to be done, so they repeated a test that DIDN'T stress the heart, and had results we ALREADY knew about.
So it's six days til her surgery, I have a patient with known heart failure, maybe shortness of breath, maybe chest pain, two non-stress tests, and an indeterminate stress test. Someone also has decided before me that a stress would be a good idea, but never really followed through. So I have six days (including two weekend days) to get her stressed (a different type of stress test) or cancel the surgery. Luckily the ladies out front (the wonderful office staff) are able to get her scheduled for early next week. I cross my fingers and let her go.
The intern asks me what happens if the stress is positive next week. Good question. If it's negative, then I'm just a worry-wort and paranoid about nothing but she should get her back fixed. If not, then they need to evaluate her to see if anything can be done to optimize her heart before her elective surgery. This may mean changing her medications, or performing a heart catheterization, or more.
Did I tell you I love clinic?
Monday, July 02, 2007
Study Says Chatty Doctors Forget Patients
Study Says Chatty Doctors Forget Patients
Funny... except for the patients. Published in the Archives of Internal Medicine via the New York Times
Funny... except for the patients. Published in the Archives of Internal Medicine via the New York Times
Sunday, July 01, 2007
Playing Doctor
I got to play "real" doctor this weekend.
Not that an anesthesiologist isn't a real doctor, but it's not immediately what comes to mind when you say doctor.
My friend volunteers at a free county medical clinic run by medical students some weekends. The medical students see patients and are staffed by physicians from the community. They were running short of physicians this week so I offered my services.
It was a little different than my usual Saturday morning, but a little fun nonetheless. I only had to ask a few questions to the "real" doctors.
A lot of me saying to medical students "just warning you... I'm an anesthesiologist."
Not that an anesthesiologist isn't a real doctor, but it's not immediately what comes to mind when you say doctor.
My friend volunteers at a free county medical clinic run by medical students some weekends. The medical students see patients and are staffed by physicians from the community. They were running short of physicians this week so I offered my services.
It was a little different than my usual Saturday morning, but a little fun nonetheless. I only had to ask a few questions to the "real" doctors.
A lot of me saying to medical students "just warning you... I'm an anesthesiologist."
Subscribe to:
Posts (Atom)
